The Pancreatic Beta Cell: Biology and Mathematics Advance Together
The human pancreas contains roughly one gram of beta cells, which secrete the hormone insulin when glucose levels rise after a meal; the insulin then returns glucose back to baseline over the course of several hours. Upon reaching baseline, insulin secretion ceases. This process is a classic example of a homeostatic negative feedback loop. In the absence of beta cells, blood glucose would fluctuate wildly with each meal and damage the body’s tissues — as is the case with type 1 diabetes, wherein the immune system kills almost all beta cells. Type 2 diabetes is more common and results from a deficiency in insulin secretion relative to the necessary amount for glucose control; this deficiency generally comes with age and weight gain and can potentially cause heart disease, dementia, blindness, peripheral neuropathy, and kidney failure. For most people, the beta cells compensate for reduced insulin efficiency by increasing insulin secretion. But when such compensation is inadequate, blood glucose levels slowly increase over many years until they reach a critical threshold and rise dramatically.
Understanding insulin secretion’s dynamic response to meals, short-term cycles of feasting and fasting, and lifelong variations in body weight is therefore crucial for diabetes treatment. Mathematical modeling has addressed two key questions in this research space: How do beta cells secrete the appropriate amount of insulin to keep glucose in the healthy range? And how does the pancreas generate the observed five-minute pulses of insulin secretion?
Experimental studies in the 1970s and 1980s revealed that beta cells respond to elevated glucose levels with bursts of action potentials: periods of spiking that alternate with periods of silence. The action potentials bring in calcium, which triggers insulin secretion. As glucose increases, the bursts become longer and the silent periods become shorter (i.e., the plateau fraction increases). But how does glucose exert this effect, and how does the increased plateau fraction lead to the secretion of more insulin? Experiments demonstrated that the regulation of electrical activity depends on the rate of glucose metabolism in the beta cell, which acts as a surrogate for blood glucose concentration. However, the link from metabolism to electrical activity and secretion remained unknown.
In 1983, the Chay-Keizer model attempted to assemble the experimental observations into a coherent, quantitative framework [1]. The voltage spikes in this model bring in calcium that slowly builds up and binds to calcium-activated potassium (KCa) channels; after many spikes, this binding process turns off the burst. Calcium pumps then reduce the calcium level once again, paving the way for the next burst. Calcium thus acts like a slow variable in a relaxation oscillator, gradually rising and falling with each period of oscillation. Researchers also determined that an adenosine triphosphate (ATP)-sensitive K+ (KATP) channel—which is closed by ATP and opened by adenosine diphosphate (ADP)—serves as the link between beta cell metabolism and increased plateau fraction. As glucose increases, KATP channel activity decreases, thus requiring more KCa channel activation and hence more calcium to terminate the bursts (see Figure 1a). The beta cell’s metabolism, which acts as a measure of blood glucose concentration, therefore increases calcium and insulin secretion by way of increased plateau fraction.
![<strong>Figure 1.</strong> Simulations with the original and augmented Chay-Keizer models compared to data. <strong>1a.</strong> In the original model, increasing glucose at \(t=30\) seconds (dashed line)—represented by reduced conductance of adenosine triphosphate (ATP)-sensitive K<sup>+</sup> (KATP) channels—increases plateau fraction and calcium. <strong>1b.</strong> Experimentally measured calcium is a square wave, not a sawtooth wave. <strong>1c.</strong> Augmented model where the endoplasmic reticulum (ER) and ATP/adenosine diphosphate (ADP) oscillate in phase with calcium. ATP/ADP does not increase when glucose increases at \(t=15\) minutes, in agreement with experiments [5]. <strong>1d.</strong> In the augmented model, oscillations persist when ER calcium uptake is blocked at \(t=15\) minutes, in agreement with experiments. Figures 1a, 1c, and 1d courtesy of the authors, and 1b courtesy of [6].](/media/iybf0tcr/figure1.jpg)
In 1987, John Rinzel demonstrated that the pattern of spikes superimposed on a plateau arises from bistability between silent and spiking states in the fast subsystem; the slow variable (calcium) carries the system cyclically between the two states (see Figures 2a and 2b). This phenomenon is called fold/homoclinic bursting because each active phase begins at a saddle node (fold) and ends at a homoclinic bifurcation. Rinzel’s work also laid the foundation for a general theory of the many types of bursting—characterized by various sets of bifurcations—that occur in different cells [9]. Eugene Izhikevich later identified over 100 distinct types of bursts, including some that had not yet been observed experimentally [4]. Additional work found that bursting in certain pituitary cells—which resembles beta cell bursting—is better fit by one of these predicted types, which is delineated by saddle node and subcritical Hopf bifurcations (see Figures 2c and 2d).
One can derive the bifurcations that are traversed during bursting—as well as their topological arrangement—by unfolding a higher codimension bifurcation [3]. Fold/homoclinic and fold/sub-Hopf bursting, along with almost all other known types, result from a codimension-four doubly-degenerate Bogdanov-Takens point [7].
Though the Chay-Keizer beta cell model is quite beautiful, it is wrong in several respects. When technology to measure calcium dynamics in cells became available, biologists learned that calcium acts like a fast variable (rather than a slow variable) in a relaxation oscillator (see Figure 1b). The Chay-Keizer model also does not account for the wide range of periods—from seconds to minutes—that are present in beta cells. Cytosolic calcium is slow compared to spike generation, but not slow enough to account for the five-minute pulses of insulin secretion.
![<strong>Figure 2.</strong> In beta cell models, bursting with spikes that appear on the plateaus is generated by a family of stable limit cycles <strong>(2a)</strong> and classified as fold/homoclinic <strong>(2b)</strong>. Bursting in certain pituitary endocrine cells looks similar <strong>(2c)</strong> but is better described by bursting models of fold/subHopf type <strong>(2d)</strong>, in which decaying transients (a “pseudo plateau”) generate the spikes. A predicted consequence is that it is very difficult to perturb the oscillations upward from silent phase to active phase [10]. Figure courtesy of the authors.](/media/fnzjfvgl/figure2.jpg)
To address these issues, researchers added two new mechanisms to the Chay-Keizer model. The first is the endoplasmic reticulum (ER): an internal reservoir of calcium that has much slower kinetics than the cytosolic calcium, thus slowing calcium oscillations and giving them the correct shape. Second, KATP channel activity was assumed not only to set the plateau fraction, but also to oscillate slowly due to oscillations in the ATP/ADP ratio (see Figure 1c). These metabolic oscillations provide another form of negative calcium feedback; when calcium levels are high, ATP is consumed to pump calcium out of the cell or into the ER, which reopens some KATP channels and subsequently terminates calcium entry.
Although glucose generally raises ATP/ADP, the mean ATP/ADP level paradoxically does not increase with glucose when the system is bursting [5]. This counterintuitive model property holds because the increased ATP production is balanced by the rise in ATP consumption to handle the larger calcium influx. The bifurcation diagram (like the one in Figure 2b but with ATP/ADP in place of calcium) reflects this effect, as the saddle-node and homoclinic bifurcations are invariant with respect to glucose. Further experimental advances eventually confirmed the predictions of the augmented Chay-Keizer model. This improved model can also accommodate the wide range of oscillation periods by varying the proportion of slow and very slow components. At last, the calcium exhibits very slow oscillations that account for the five-minute pulses of insulin secretion.
However, Sandra Postić and her colleagues recently challenged this hard-won synthesis of experimentation and modeling with new data and proposed an alternative mechanism in which beta cell oscillations are governed by the release of calcium from the ER — not by outside entry through plasma membrane ion channels [8]. In their study, the stimulation of calcium release triggered oscillations in basal glucose, while the inhibition of release suppressed oscillations when glucose was just above the threshold. The authors concluded that calcium release is both necessary and sufficient for oscillations, and relegated calcium entry to a subordinate role of refilling the ER.
Utilizing the long history of oscillation modeling based on calcium release, we rebutted this recent work and argued that the calcium release mechanism is at odds with existing data [2]. If the calcium that raises cytosolic calcium levels comes from the ER, then the two calcium pools would be out of phase (contrary to experiments). The canonical calcium entry model exhibits the correct behavior (see Figure 1c). The release model in [8] also predicts that depletion of the ER will terminate oscillations, which does not occur experimentally. However, the canonical model again gets this right due to the redundancy of ER and ATP/ADP mechanisms (see Figure 1d). We also confirmed that the canonical model can account for the new data.
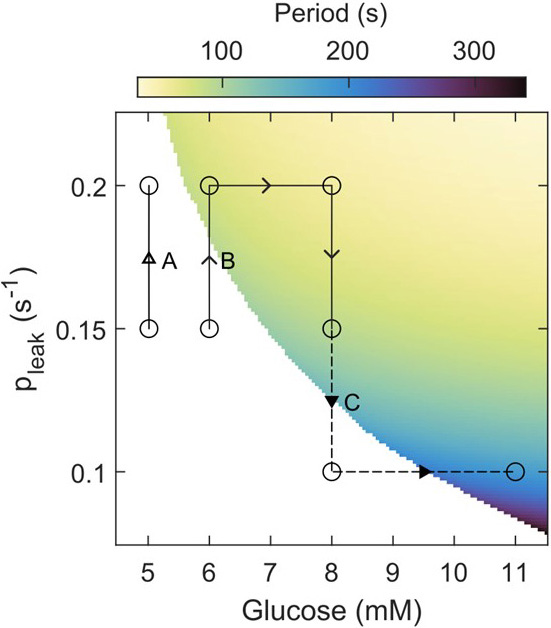
To its credit, Postić’s recent study drew attention to the range of glucose where most of life is spent: just below and above the threshold [8]. But as a corollary, small ionic currents cause major effects in that regime. Though such currents can shift the threshold for electrical activity, this threshold is primarily set by the KATP channels that act as gatekeepers for calcium entry. We hence concluded that calcium release is neither necessary nor sufficient for calcium oscillations (see Figure 3).
A combination of mathematics and biological experimentation has successfully addressed a plethora of specific problems that pertain to beta cell oscillations. Moreover, the stunning diversity of oscillation patterns derives from a simple, unified framework in which a relatively small number of mechanisms quantitatively combine in different proportions. We believe that the pleasing concordance between the model and various phenomena arises because cells encounter the previously identified bifurcations as they randomly mutate, and the bifurcations that prove useful are fixed by natural selection.
References
[1] Chay, T.R., & Keizer, J. (1983). Minimal model for membrane oscillations in the pancreatic beta-cell. Biophys. J., 42(2), 181-190.
[2] Fletcher, P.A., Thompson, B., Liu, C., Bertram, R., Satin, L.S., & Sherman, A.S. (2023). Ca2+ release or Ca2+ entry, that is the question: What governs Ca2+ oscillations in pancreatic β cells? Am. J. Physiol. Endocrinol. Metab., 324(6), E477-E487.
[3] Golubitsky, M., Josić, K., & Kaper, T.J. (2001). An unfolding theory approach to bursting in fast-slow systems. In H.W. Broer, B. Krauskopf, & G. Vegter (Eds.), Global analysis of dynamical systems (pp. 277-308). Boca Raton, FL: CRC Press.
[4] Izhikevich, E.M. (2000). Neural excitability, spiking and bursting. Int. J. Bifurcat. Chaos, 10(6), 1171-1266.
[5] Marinelli, I., Thompson, B.M., Parekh, V.S., Fletcher, P.A., Gerardo-Giorda, L., Sherman, A.S., … Bertram, R. (2022). Oscillations in K(ATP) conductance drive slow calcium oscillations in pancreatic β-cells. Biophys. J., 121(8), 1449-1464.
[6] Nunemaker, C.S., Bertram, R., Sherman, A., Tsaneva-Atanasova, K., Daniel, C.R., & Satin, L.S. (2006). Glucose modulates [Ca2+]i oscillations in pancreatic islets via ionic and glycolytic mechanisms. Biophys. J., 91(6), 2082-2096.
[7] Osinga, H.M., Sherman, A., & Tsaneva-Atanasova, K. (2012). Cross-currents between biology and mathematics: The codimension of pseudo-plateau bursting. Discrete Contin. Dyn. Syst., 32(8), 2853-2877.
[8] Postić, S., Sarikas, S., Pfabe, J., Pohorec, V., Bombek, L.K., Sluga, N., … Rupnik, M.S. (2023). High-resolution analysis of the cytosolic Ca2+ events in β cell collectives in situ. Am. J. Physiol. Endocrinol. Metab., 324(1), E42-E55.
[9] Rinzel, J. (1987). A formal classification of bursting mechanisms in excitable systems. In E. Teramoto & M. Yumaguti (Eds.), Mathematical topics in population biology, morphogenesis and neurosciences: Proceedings of an international symposium held in Kyoto, November 10-15, 1985 (pp. 267-281). New York, NY: Springer-Verlag.
[10] Stern, J.V., Osinga, H.M., LeBeau, A., & Sherman, A. (2008). Resetting behavior in a model of bursting in secretory pituitary cells: Distinguishing plateaus from pseudo-plateaus. Bull. Math. Biol., 70(1), 68-88.
About the Authors
Arthur S. Sherman
Applied Mathematician, National Institutes of Health
Arthur S. Sherman is an applied mathematician at the National Institutes of Health who studies beta cells and other biological systems.
Patrick A. Fletcher
Applied Mathematician, National Institutes of Health
Patrick A. Fletcher is an applied mathematician at the National Institutes of Health who studies beta cells and other biological systems.
Richard Bertram
Professor, Florida State University
Richard Bertram is a professor in the Department of Mathematics and a graduate faculty member in the Molecular Biophysics Program and the Neuroscience Program at Florida State University.
Leslie S. Satin
Beta cell electrophysiologist, University of Michigan
Leslie S. Satin is a beta cell electrophysiologist at the University of Michigan.
Stay Up-to-Date with Email Alerts
Sign up for our monthly newsletter and emails about other topics of your choosing.



